Health workers are central to the COVID-19 pandemic response, balancing additional service delivery needs while preserving access to essential health services and deploying COVID-19 vaccines. They also face higher risks of infection in their efforts to protect the greater community and are exposed to hazards such as psychological distress, fatigue and stigma.
To help policy-makers and planners invest in ensuring the readiness, education and learning of the health workforce, WHO provides support for strategic workforce planning, support and capacity-building.
- 1. Interim guidance on Health workforce policy and management in the context of the COVID-19 pandemic response.
- 2. Health Workforce Estimator to anticipate response staffing requirements
- 3. The Health Workforce Support and Safeguards List comprises countries facing the most pressing health workforce challenges, from which active international recruitment is discouraged.
Dedicated learning resources to support expanded clinical roles and tasks, as well as support for COVID-19 vaccines roll-out, are available for individual health workers. Managers and planners can access additional resources to support learning and education requirements.
- Open WHO has a multi-language course library that is also accessible through the WHO Accdemacy COVID-19 learning app, which includes a new augmented reality course on personal protective equipment.
- The COVID-19 Vaccine Introduction Toolbox has the latest resources, including guidance, tools and trainings.
Learn how to utilise your role as a health worker and trusted source of information. You can also be a role model by getting the vaccine, protecting yourself and helping your patients and the public understand the benefits.
- Review WHO information network for Epidemics updates for accurate information and clear explanations about COVID-19 and vaccines.
- Access the community engagement guide for tips and discussion topics to be considered in vaccine delivery and demand.
- Learn about infodemic management: help your patients and communities manage the overabundance of information and learn how to seek trusted sources.
- Diagnostic testing for SARS-CoV-2 infection; Use of the antigen detection; Different tests for COVID-19
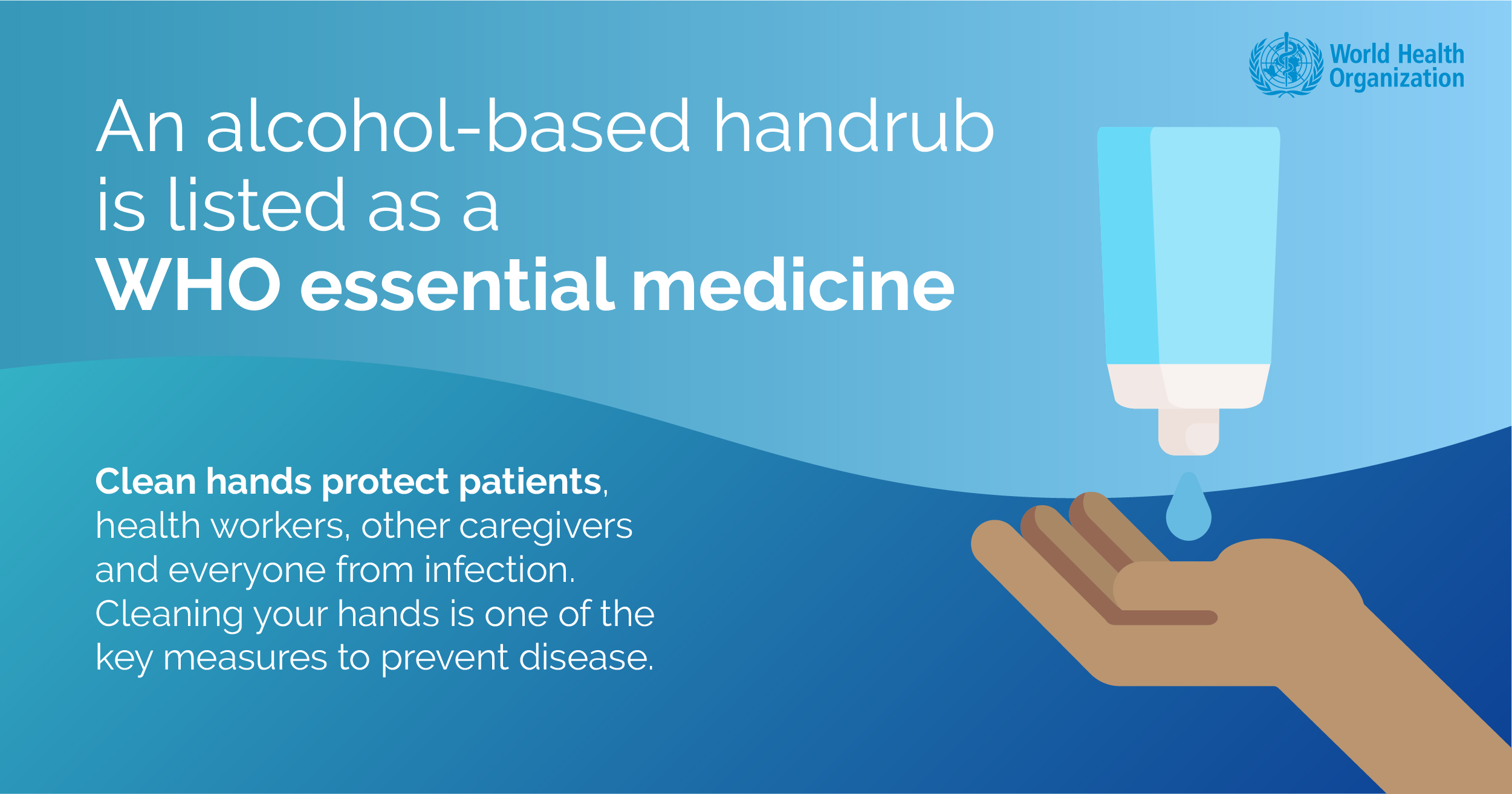

Infection prevention and control
Preventing SARS-CoV-2 infections in health workers requires a multi-pronged, integrated approach of infection prevention and control (IPC) and occupational health and safety (OHS) measures. WHO recommends that all healthcare facilities establish and implement IPC programmes and OHS programmes with protocols that ensure health worker safety and prevent infections with SARS-CoV-2 in the work environment.
A blame-free system for managing health worker exposures to COVID-19 should be in place to promote and support reporting of exposures or symptoms. Health workers should be encouraged to report both occupational and non-occupational exposures to COVID-19.
Occupational safety and health
This document provides specific measures to protect occupational health and safety of health workers and highlights the duties, rights and responsibilities for health and safety at work in the context of COVID-19.
Prevention of violence
Measures for zero-tolerance of violence should be established in all health facilities and for protection of health workers in the community. Workers should be encouraged to report incidences of verbal, physical violate and sexual harassment. Security measures, including guards, panic buttons, cameras should be introduced. Staff should be trained in prevention of violence.

Prevention of fatigue
Develop working time schemes for the scheme for the different categories of health workers involved - ICUs, primary care, first responders, ambulances, sanitation etc., including maximum working hours per work shift (five eight-hours or four 10-hour shifts per week), frequent rest breaks (e.g. every 1-2 hours during demanding work) and minimum 10 consecutive hours of rest between work shifts.
Compensation, hazard pay, priority treatment
Excessive hours of work should be discouraged. Ensure adequate staffing levels to prevent excessive individual workloads, and minimize the risk of unsustainable working hours. Where extra hours are necessary, compensatory measures such as overtime pay or compensatory time off should be considered. Where necessary, and in a gender-sensitive manner, consideration should be given to mechanisms for determining hazardous duty pay. Where exposure and infection are work-related, health and emergency workers should be provided with adequate compensation, including when quarantined. In the event of scarcity of treatment for those contracting COVID19, each employer should develop, through social dialogue, a treatment distribution protocol and specify the priority of health and emergency workers in receiving treatment.
Post time: Jun-25-2021
